Apigenin ameliorates HFD-induced NAFLD through regulation of
<p> </p>
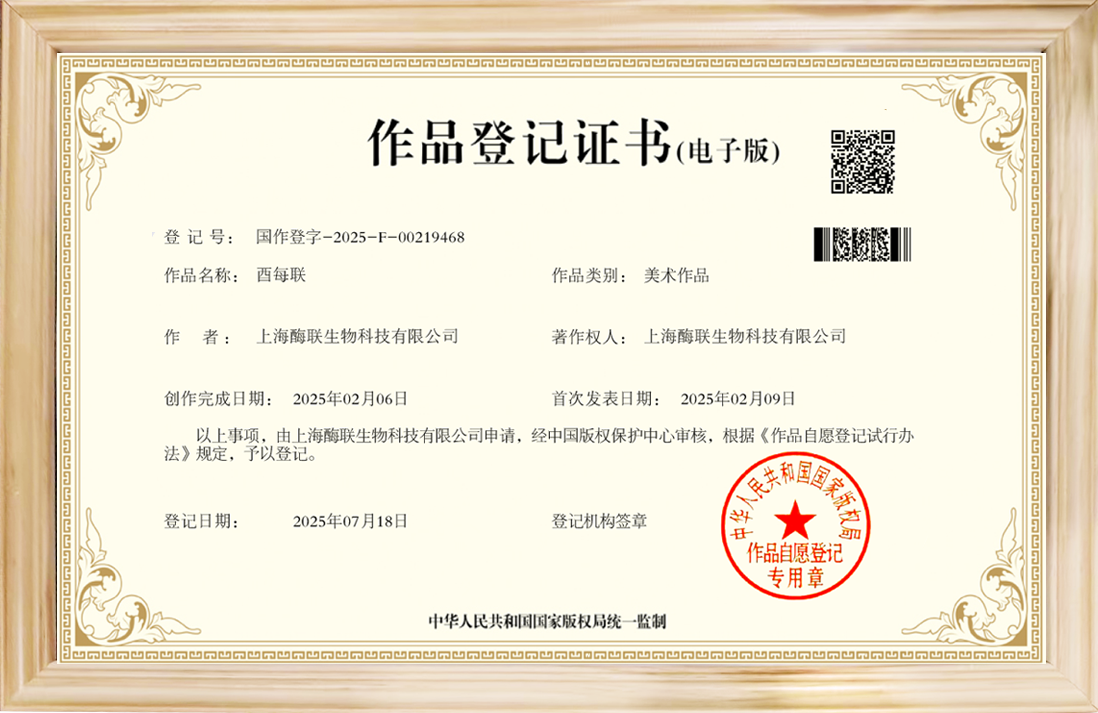
<p><b>“上海酶联文献” </b><strong>Acknowledgments</strong></p>
<p>This work was supported by the National Key R&D Program (2016YFD0501009 and 2016YFD0501200), the Natural Science Foundation of Jiangsu Province (BK20161452), the Fundamental Research Funds for the Central Universities (KYZ201848), the Priority Academic Program Development of Jiangsu Higher Education Institutions, the NAU International Cooperation and Cultivation Project (2018-AF-20) and the Key Program of Science and Technology Planning of Guangdong Province (2017B020202010).</p>
<p>Declaration of Competing Interest</p>
<p>The authors declare no conflicts of interest.</p>
<p><strong>References</strong></p>
<p>[1]Ahmed MH. Non-alcoholic fatty liver disease (NAFLD): new challenge for general practitioners and important burden for health authorities? Prim Care Diabetes 2010;4:129–37.</p>
<p>[2]Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol 2013;10:686–90.</p>
<p>[3]Karlas T, Wiegand J, Berg T. Gastrointestinal complications of obesity: non-alcoholic fatty liver disease (NAFLD) and its sequelae. Best Pract Res Clin Endocrinol Metab 2013;27:195–208.</p>
<p>[4]Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol 2015;62:S47–64.</p>
<p>[5]Birkenfeld AL, Shulman GI. Non alcoholic fatty liver disease, hepatic insulin resistance and type 2 diabetes. Hepatology 2014;59:713–23.</p>
<p>[6]Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol 2016;65:589–600.</p>
<p>[7]Mantovani A, Zaza G, Byrne CD, Lonardo A, Zoppini G, Bonora E, et al. Nonalcoholic fatty liver disease increases risk of incident chronic kidney disease: a systematic review and meta-analysis. Metabolism Clinical & Experimental 2017;79:64–76.</p>
<p>[8]Dietrich MO, Horvath TL. Limitations in anti-obesity drug development: the critical role of hunger-promoting neurons. Nat Rev Drug Discov 2012;11:675–91.</p>
<p>[9]Harris CM, Massey V. The oxidative half-reaction of xanthine dehydrogenase with NAD; reaction kinetics and steady-state mechanism. J Biol Chem 1997;272: 28335–41.</p>
<p>[10]Cheung KJ, Iphigenia T, Pavlos P, Ilsa R, Oksana G, Toshio O, et al. Xanthine oxidoreductase is a regulator of adipogenesis and PPARgamma activity. Cell Metab 2007;5:115–28.</p>
<p>[11]Kushiyama A, Okubo H, Sakoda H, Kikuchi T, Fujishiro M, Sato H, et al. Xanthine oxidoreductase is involved in macrophage foam cell formation and atheroscle-rosis development. Arterioscler Thromb Vasc Biol 2012;32:291–8.</p>
<p>[12]Kurosaki M, Calzi ML, Scanziani E, Garattini E, Terao M. Tissue- and cell-specific expression of mouse xanthine oxidoreductase gene in vivo: regulation by bacterial lipopolysaccharide. Biochem J 1995;306:225–34.</p>
<p>[13]Xu C, Wan X, Xu L, Weng H, Yan M, Miao M, et al. Xanthine oxidase in non-alcoholic fatty liver disease and hyperuricemia: one stone hits two birds. J Hepatol 2015;62:1412–9.</p>
<p>[14]Lanaspa MA, Sanchez-Lozada LG, Yea-Jin C, Christina C, Mehmet K, Roncal-Jimenez CA, et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: potential role in fructose-dependent and -independent fatty liver. J Biol Chem 2012;287:40732–44.</p>
<p>[15]Li Y, Xu C, Yu C, Xu L, Miao M. Association of serum uric acid level with non-alcoholic fatty liver disease: a cross-sectional study. J Hepatol 2009;50:1029–34.</p>
<p>[16]Wang B, Yang RN, Zhu YR, Xing JC, Lou XW, He YJ, et al. Involvement of xanthine oxidase and paraoxonase 1 in the process of oxidative stress in nonalcoholic fatty liver disease. Mol Med Rep 2016;15:387–95.</p>
<p>[17]Wree A, Mcgeough MD, Peña CA, Schlattjan M, Li H, Inzaugarat ME, et al. NLRP3 inflammasome activation is required for fibrosis development in NAFLD. J Mol Med 2014;92:1069–82.</p>
<p>[18]Dixon LJ, Flask CA, Papouchado BG, Feldstein AE, Nagy LE. Caspase-1 as a central regulator of high fat diet-induced non-alcoholic steatohepatitis. PLoS One 2013;8: e56100.</p>
<p>[19]Szabo G, Csak T. Inflammasomes in liver diseases. J Hepatol 2012;57:642–54.</p>
<p>[20]Jan P, Shashi B, Timea C, Dora L, Karen K, Victoria M, et al. IL-1 receptor antagonist ameliorates inflammasome-dependent alcoholic steatohepatitis in mice. J Clin Investig 2012;122:3476–89.</p>
<p>[21]Dixon LJ, Michael B, Samjhana T, Papouchado BG, Feldstein AE. Caspase-1-mediated regulation of fibrogenesis in diet-induced steatohepatitis. Lab Invest 2012;92:713–23.</p>
<p>[22]Schroder K, Tschopp J. The Inflammasomes. Cell 2010;140:821–32.</p>
<p>[23]Gyongyi S, Jan P. Inflammasome activation and function in liver disease. Nat Rev Gastroenterol Hepatol 2015;12:387–400.</p>
<p>[24]Lozovoy MA, Simão AN, Panis C, Rotter MA, Reiche EM, Morimoto HK, et al. Oxidative stress is associated with liver damage, inflammatory status, and corticosteroid therapy in patients with systemic lupus erythematosus. Lupus 2011;20:1250–9.</p>
<p>[25]Annette I, Johji N, Fabio M, Thierry R, Didier LR, Miner JN, et al. Xanthine oxidoreductase regulates macrophage IL1β secretion upon NLRP3 inflammasome activation. Nat Commun 2015;6:6555.</p>
<p>[26]Mohamed L. Emerging inflammasome effector mechanisms. Nat Rev Immunol 2011;11:213–20.</p>
<p>[27]Wan X, Xu C, Lin Y, Lu C, Li D, Sang J, et al. Uric acid regulates hepatic steatosis and insulin resistance through the NLRP3 inflammasome-dependent mechanism. J Hepatol 2016;64:925–32.</p>
<p>[28]And KHM, Mohamed S. Flavonoid (myricetin, quercetin, kaempferol, luteolin, and apigenin) content of edible tropical plants. Journal of Agricultural & Food Chemistry 2001;49:3106–12.</p>
<p>[29]Feng X, Wen Y, Li X, Zhou F, Zhang W, Qi S, et al. Apigenin, a modulator of PPARγ, attenuates HFD-induced NAFLD by regulating hepatocyte lipid metabolism and oxidative stress via Nrf2 activation. Biochem Pharmacol 2017:136–49.</p>
<p>[30]Je-Hyuk L, Yu ZH, So Yean C, Yeong Shik K, Soo LY, Choon Sik J. Anti-inflammatory mechanisms of apigenin: inhibition of cyclooxygenase-2 expression, adhesion of monocytes to human umbilical vein endothelial cells, and expression of cellular adhesion molecules. Arch Pharm Res 2007;30:1318–27.</p>
<p>[31]Shao H, Jing K, Mahmoud E, Huang H, Fang X, Yu C. Apigenin sensitizes colon cancer cells to antitumor activity of ABT-263. Mol Cancer Ther 2013;12: 2640–50.</p>
<p>[32]Li R, Wang X, Qin T, Qu R, Ma S. Apigenin ameliorates chronic mild stress-induced depressive behavior by inhibiting interleukin-1β production and NLRP3 inflammasome activation in the rat brain. Behav Brain Res 2016;296: 318–25.</p>
<p>[33]Mafuyu O, Ko F. Antiadipogenic effect of dietary apigenin through activation of AMPK in 3T3-L1 cells. J Agric Food Chem 2011;59:13346–52.</p>
<p>[34]Kim MA, Kang K, et al. Apigenin isolated from Daphne genkwa Siebold et Zucc. Inhibits 3T3-L1 preadipocyte differentiation through a modulation of mitotic clonal expansion. Life Sci 2014;101:64–72.</p>
<p>[35]Carlos E, Veronica N, Nathan LP, Verena C, Ana PG, Maria Thereza B, et al. Flavonoid apigenin is an inhibitor of the NAD+ ase CD38: implications for cellular NAD+ metabolism, protein acetylation, and treatment of metabolic syndrome. Diabetes 2013;62:1084–93.</p>
<p>[36]Cui Y, Wang Q, Li X, Zhang X. Experimental nonalcoholic fatty liver disease in mice leads to cytochrome p450 2a5 upregulation through nuclear factor erythroid 2-like 2 translocation. Redox Biol 2013;1:433–40.</p>
<p>[37]Tu K, Zheng X, Yin G, Zan X, Yao Y, Liu Q. Evaluation of Fbxw7 expression and its correlation with expression of SREBP-1 in a mouse model of NAFLD. Mol Med Rep 2012;6:525–30.</p>
<p>[38]Tongfang T, Yongheng S, Min L, Zhiping L, Jing H. Pro-inflammatory activated Kupffer cells by lipids induce hepatic NKT cells deficiency through activation-induced cell death. PLoS One 2013;8:e81949.</p>
<p>[39]disease Katherine S Liver. Kupffer cells regulate the progression of ALD and NAFLD. Nat Rev Gastroenterol Hepatol 2013;10:503.</p>
<p>[40]Zhang X, Zhang JH, Chen XY, Hu QH, Wang MX, Jin R, et al. ROS-induced TXNIP drives fructose-mediated hepatic inflammation and lipid accumulation through NLRP3 inflammasome activation. Antioxid Redox Signal 2015;22:848–70.</p>
<p>[41]Mridha AR, Wree A, Robertson AAB, Yeh MM, Johnson CD, Rooyen DMV, et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol 2017;66:1037–46.</p>
<p>[42]Marí-Carmen D, Miguel A, Rafael M, José MV, Máximo V, Pallardó FV, et al. Xanthine oxidase is involved in free radical production in type 1 diabetes: protection by allopurinol. Diabetes 2002;51:1118–24.</p>
<p>[43]Juanwen Z, Chengfu X, Ying Z, Yu C. The significance of serum xanthine oxidoreductase in patients with nonalcoholic fatty liver disease. Clin Lab 2014; 60:1301–17.</p>
<p>[44]Kato S, Kawase T, Alderman J, Inatomi N, Lieber CS. Role of xanthine oxidase in ethanol-induced lipid peroxidation in rats. Gastroenterology 1990;98:203–10.</p>
<p>[45]Feng X, Weng D, Zhou F, Owen YD, Qin H, Zhao J, et al. Activation of PPARγ by a natural flavonoid modulator, Apigenin ameliorates obesity-related inflammation via regulation of macrophage polarization. EBioMedicine 2016;9:61–76.</p>
<p>[46]Lin CM, Chen CS, Chen CT, Liang YC, Lin JK. Molecular modeling of flavonoids that inhibits xanthine oxidase. Biochem Biophys Res Commun 2002;294:167–72.</p>
<p>[47]Tilg H, Moschen AR. IL-1 cytokine family members and NAFLD: neglected in metabolic liver inflammation. J Hepatol 2011;55:960–2.</p>
<p>[48]Qi J, Sun LQ, Qian SY, Yu BY. A novel multi-hyphenated analytical method to simultaneously determine xanthine oxidase inhibitors and superoxide anion scavengers in natural products. Anal Chim Acta 2017;984:124–33.</p>
<p>[49]Chen T, Li L, Lu X, Jiang H, Su Z. Absorption and excretion of luteolin and apigenin in rats after oral administration of Chrysanthemum morifolium extract. Journal of Agricultural & Food Chemistry 2009;55:273–7.</p>
<p><strong>Y. Lv et al. / Journal of Nutritional Biochemistry 71 (2019) 110–121 121</strong></p>
<p>[50]Mo S, Zhou F, Lv Y, Hu Q, Kong L. Hypouricemic action of selected flavonoids in mice: structure-activity relationships. Biol Pharm Bull 2007;30:1551–6.</p>
<p>[51]Lepley DM, Li B, Birt DF, Pelling JC. The chemopreventive flavonoid apigenin induces G2/M arrest in keratinocytes. Carcinogenesis 1996;17:2367–75.</p>
<p>[52]Ali F, Rahul Naz F, Jyoti S, Siddique YH. Health functionality of apigenin: a review. International Journal of Food Properties 2017;20:1197–238.</p>
<p>[53]Leemans JC, Cassel SL, Sutterwala FS. Sensing damage by the NLRP3 inflamma-some. Immunol Rev 2011;243:152–62.</p>
<p>[54]Broderick L, De ND, Franklin BS, Hoffman HM, Latz E. The Inflammasome and autoinflammatory syndromes. Annu Rev Pathol 2014;10:395–424.</p>
<p>[55]Wree A, Broderick L, Canbay A, Hoffman HM, Feldstein AE. From NAFLD to NASH to cirrhosis-new insights into disease mechanisms. Nat Rev Gastroenterol Hepatol 2013;10:627–36.</p>
<p>[56]Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med 2011;17:179–88.</p>
<p>[57]Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature 2010;464:1357–61.</p>
<p>[58]Masters SL, Dunne A, Subramanian SL, Hull RL, Tannahill GM, Sharp FA, et al. Activation of the NLRP3 inflammasome by islet amyloid polypeptide provides a mechanism for enhanced IL-1β in type 2 diabetes. Nat Immunol 2010;11: 897–904.</p>
<p>Henaomejia J, Elinav E, Jin C, Hao L, Mehal WZ, Strowig T, et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature 2012;482:179–85. </p>


 酶联官方手机二维码
酶联官方手机二维码